‘A pregnant woman is normally not a sick person when she arrives at the facility. But she can become sick if she gets there too late, or if the provider can’t give her the support she needs at that time.’
Maureen is a nurse midwife working within the maternity wards of a primary (or Level 3) health facility in Kakamega, a county on Kenya’s Western border. Her interaction with mothers begins at the start of their pregnancy – ‘the earlier the better’ – first through antenatal care (ANC) check-ups, then delivery, and extending to postnatal care. ‘If you manage a mum well during ANC, you reduce her risk of complications during delivery.’ she explains, adding ‘I find this very fulfilling’.
But she also identifies a number of challenges her facility has faced, including patients not turning up for prenatal care and providers lacking the right skills and equipment to deal with maternal complications and emergencies as they happen. In Kakamega, where Maureen lives and works, the current delivery care model means that most women choose to give birth in convenient facilities nearby – predominantly primary care centers like Maureen’s – with referrals to higher-level facilities offered only when complications develop – when it’s often too late.

Jacaranda Health and a coalition of Kenya-based partners are undertaking a Service Delivery Redesign project with an ambitious goal; to reorganize the county’s health services so that all deliveries take place in advanced facilities equipped to deal with emergencies. Achieving this means that the services that support a mother throughout her journey are coordinated, high quality, and seamlessly integrate within existing networks of care.
Maureen is a mentor within Jacaranda’s MENTORS program, a peer-to-peer model that empowers government providers with critical emergency care skills to champion high quality maternal and newborn care in their respective facilities. ‘The program has changed the way care is delivered to mothers’, says Maureen. ‘Just the other day we delivered an asphyxiated baby from a first-time mother. It was floppy, and had a very weak pulse. We applied our program knowledge until oxygen saturation was higher, and its pulse was stable. We discharged mother and baby knowing we had saved a life and the burden of grief from losing a baby.’
The MENTORS program forms a part of the wider picture for SDR. Mothers not only need to receive high quality care when they reach the facility, but also know when to seek this care, where to go, and be rapidly referred if she develops early signs of complications. The project therefore brings together a package of evidence-based solutions that ‘plug-into’ a mother’s journey through the health system.
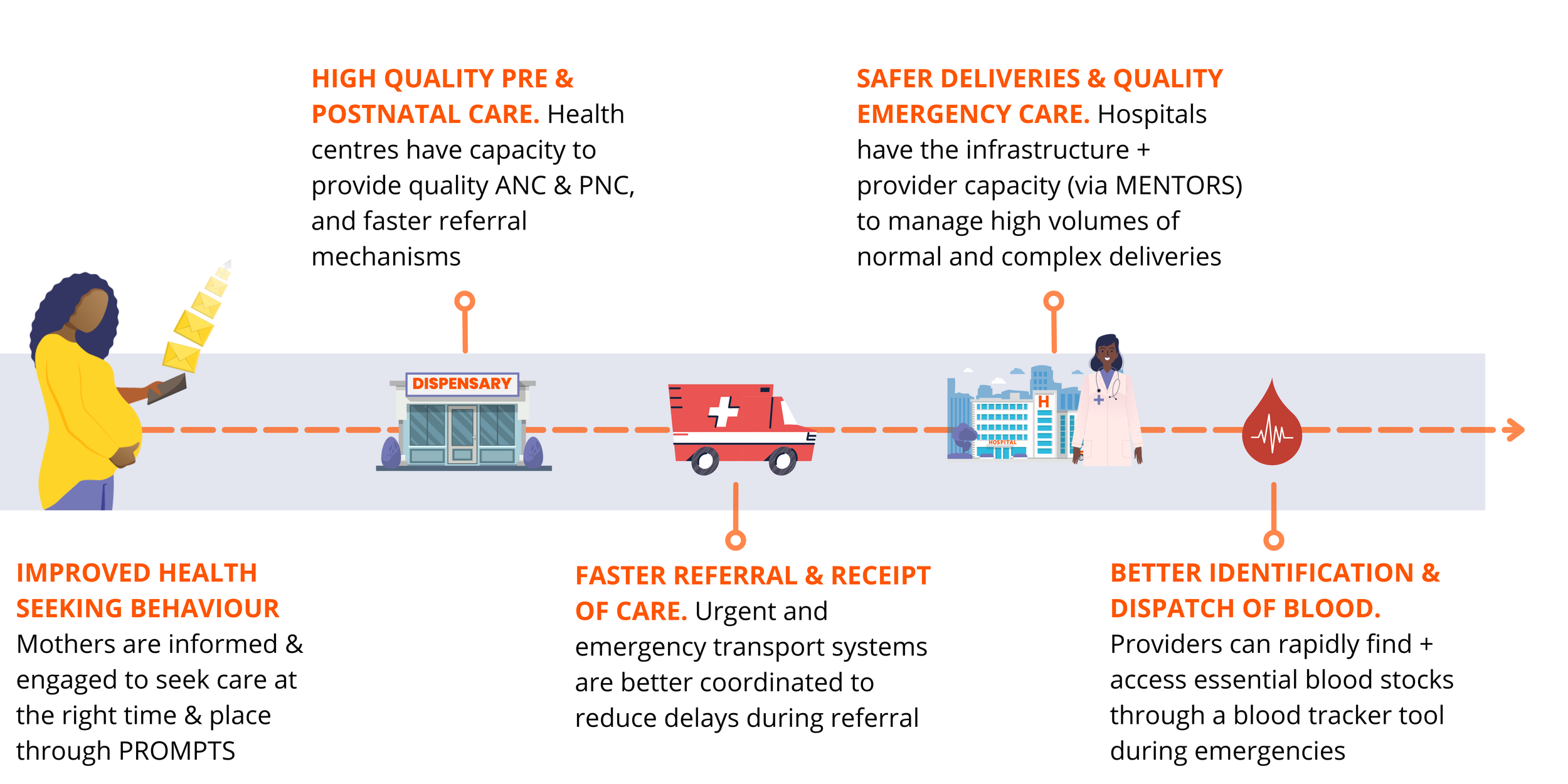
Maureen explains that because of PROMPTS, Jacaranda’s SMS-based digital health tool, mothers are more routinely attending ANC (thanks to appointment reminders they receive through the platform), as well as holding providers to account by sharing their feedback on issues like respectful care, and whether all the necessary clinical steps were performed. ‘Our patients are now being asked how they were treated [through PROMPTS], and we use their feedback to monitor and improve our attitudes.’ She explains, ‘Mothers in the community have really started to embrace our services as a result.’
Similarly, Rescue – an emergency transport dispatch service – closes the loop by ensuring mothers in need can be rapidly connected with available, qualified, and trained emergency transportation (bodas, taxis, ambulances) – whether coming from home, or referred from a lower to higher-level facility. ‘Thanks to [MENTORS], myself and colleagues are able to recognize early signs of complications and get these mothers to the nearest hospital (Level 4 or 5) in minutes by calling Rescue. They’re so quick and efficient. We know our clients are in safe hands’.
Only last week, Maureen saw this integrated service come together to save a life.
‘We had a sixteen year old girl delivering a baby. She was scared, but had received the messages [from PROMPTS] about what to bring with her during delivery. Unfortunately, during delivery she bled a lot. We applied all that we have learnt [through MENTORS], and could effectively stall the bleeding. We called Rescue, who were on-hand in minutes in case a referral was needed. Luckily, we delivered the baby and saved the life of this girl.’
Successful redesign in Kakamega will see all deliveries redirected to Level 4 & 5 facilities equipped to deliver quality care; to achieve this – and meet a shift in the demand for care – we recognize that hospitals need well-trained providers on the ground, the infrastructure and resources to deliver care consistently, and capacity to offer definitive care for complications like that of Maureen’s patient. Better health system efficiency will mean better health outcomes for the women relying on a coordinated health system to deliver their babies. ‘There is no reason that we should lose a life.’ Maureen concludes. ‘With competent midwives, the right equipment, and faster referral systems, we don’t need to lose a mother over a preventable issue.’